Jan 16, 2023
Sexually transmitted infections (STIs) and how you can get them
We get it: sexually transmitted infections (STIs) aren’t the sexiest thing to think about. But they’re nothing to be ashamed of and probably more common than you think! About 1 in 6 Australians are diagnosed with an STI in their lifetime, and worldwide, more than 1 million STIs are acquired every day. So, if you’re having sex with another person, let’s all agree to do it safely, shall we?
What is an STI and how is it acquired?
The name gives it away – sexually transmitted infections are primarily passed between people during sexual intercourse. However, some STIs are contractable through skin-to-skin contact. STIs aren’t hereditary, although, some can be passed on from mother to baby during pregnancy, delivery and breastfeeding.
You can’t tell if someone has an STI by looking at them, so it’s important for you and any sexual partner/s to know if you’re at risk of contracting an infection.
What are the common STIs?
With so many acronyms and tricky names, it’s no wonder there’s often confusion around STIs. There are three types of STIs: bacterial STIs, viral STIs, and one parasitic STI. Of these, there are eight pathogens (otherwise known as microorganisms that can cause infection or disease) that are linked to STIs.
- Bacterial STIs: These can generally be treated and cured by antibiotics.
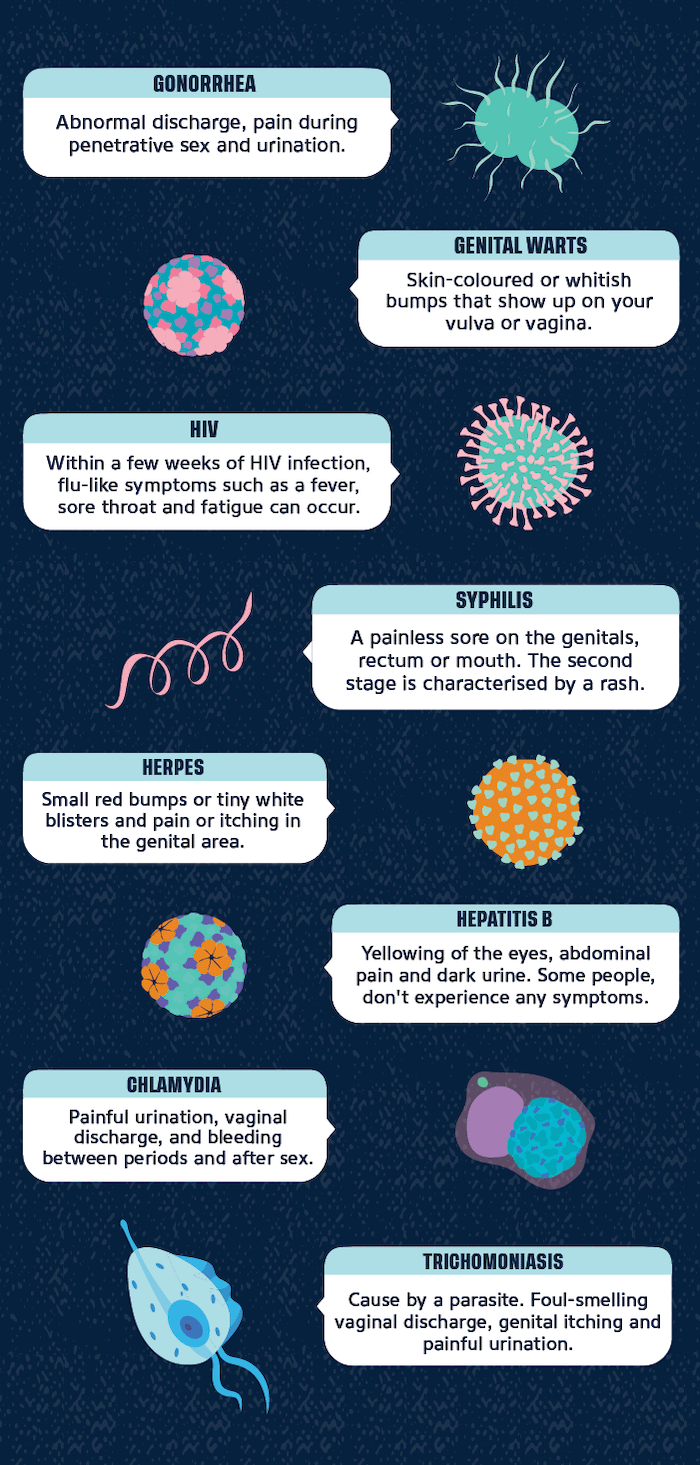
- Gonorrhoea: Abnormal discharge, pain during penetrative sex and urination.
- Chlamydia: Painful urination, vaginal discharge, and bleeding between periods and after sex.
- Syphilis: A painless sore on the genitals, rectum or mouth. The second stage is characterised by a rash.
- Viral STIs: While these STIs can be managed, unfortunately, there’s currently no cure. You’ll likely be prescribed an antiviral drug to keep the infection in check, but you might still carry and be able to pass on the virus.
- Hepatitis B: Yellowing of the eyes, abdominal pain and dark urine. Some people don’t experience any symptoms.
- Herpes simplex virus (HSV): Small red bumps or tiny white blisters, and pain or itching in the genital area.
- Human immunodeficiency virus (HIV): Within a few weeks of HIV infection, flu-like symptoms such as fever, sore throat and fatigue can occur.
- Human papillomavirus (HPV): Skin-coloured or whitish bumps that show up on your vulva or vagina.
- Parasitic STI:
- Trichomoniasis: Foul-smelling vaginal discharge, genital itching and painful urination. An oral antibiotic is effective at treating trichomoniasis.
What are the most common STI symptoms?
Many STIs are considered ‘asymptomatic’ because the symptoms generally aren’t noticeable. That’s why it’s super important to get regular checks even if you aren’t experiencing STI symptoms. If a person is infected, it’s possible for them to pass on the STI, regardless of whether or not they have symptoms.
The symptoms linked to some STIs which you should keep an eye out for, include:
- Warts, lumps, rashes, blisters, or swelling
- Pain during sex
- Pain passing urine
- Unusual vaginal discharge
- Painful, irregular periods and/or bleeding between periods or after sex
- Itching or soreness of the genitals
- Abdominal pain
Many of these symptoms are similar to other conditions, such as urinary tract infections (UTIs), so as a general rule if you’re experiencing any symptoms that are unusual for you, it’s important to discuss them with your GP or medical professional. Untreated STIs can lead to other serious health conditions or develop into sexually transmitted diseases (STDs).
What’s the difference between an STD and STI?
You’ve probably heard ‘STD’ and ‘STI’ being used interchangeably. Although they broadly refer to the same thing, making a distinction between them helps reduce the stigma around STIs. An STI is when you have an infection but you may not be experiencing symptoms. An STD is when you have symptoms.
Many STIs can be cured or treated before they become STDs. If an STI becomes an STD, possible symptoms include:
- Fever
- Recurring pain
- Fatigue
- Memory loss
- Changes to vision or hearing
- Nausea
- Weight loss
- Lumps or swelling
Again, if you notice any symptoms that are out of the ordinary, it’s important to book an appointment with your GP or medical professional.
What are the best ways to prevent an STI?
- Awareness: Knowing about the risks of STIs helps you make informed decisions.
- Communication: Talk honestly and thoughtfully with any sexual partner/s about whether you or they have an STI. If in doubt, you should both have an STI check with a GP or medical professional before having sex. It might be awkward, but it’s better to be on the safe side.
- Protection: Consistently and correctly using contraceptive barriers such as condoms and diaphragms are your best physical defence to prevent passing on or acquiring an STI.
- Act proactively: If you are sexually active, it’s smart to have regular STI checks as recommended by your GP or medical professional. This is particularly important if you know your sexual partner/s is involved with other people. If there’s any chance you could have acquired an STI, discuss it with your GP or medical professional – don’t wait for symptoms.
Safe sex is the best STI prevention
Having sex is a fun part of life, however, it does come with responsibility. Practising safe sex to reduce the risk of passing on or acquiring an STI is essential for you and your partner/s. Lastly, if you do contract an STI, don’t stress - you’re not alone and you shouldn’t feel embarrassed.
Love, Libra x
Essity makes no warranties or representations regarding the completeness or accuracy of the information. This information should be used only as a guide and should not be relied upon as a substitute for professional, medical or other health professional advice.